ADHD and insomnia: why can't I sleep or relax or focus or sleep or...
ADHD is comorbid with many psychiatric diseases - among them, sleep disorders are very common. One study found insomnia disorder in 44% of adults with ADHD (Fadeuilhe et. al, 2021). In another Australian study, 62% of children with ADHD had sleep issues, and around a third of those took sleep medications(Efron et al. 2014). In the general population, studies find different rates of insomnia, but typically between 10-30% (Morin et. al, 2020). It’s difficult to determine whether issues with sleep are an intrinsic symptom of ADHD, or whether insomnia leads to an exacerbation of ADHD-like symptoms. Some researchers argue that as disordered sleep manifests itself in insomnia-like symptoms, it can easily lead to misdiagnosis (Owens, 2008). Essentially, troubles sleeping lead to cognitive and emotional issues, which is also a hallmark sign of ADHD. We’ve all experienced this - when you have a poor night’s sleep, you’re much more likely to experience big mood swings, feel like you can’t think or focus, and maybe just be a bit grumpy overall.
This scenario isn’t entirely dissimilar to having ADHD. This raises one concern - it’s possible that a child who has a sleep disorder gets misdiagnosed with ADHD. However, although this can happen, it doesn’t explain the entirety of the relationship between the two. It’s uncertain what exactly the relationship between sleep issues and ADHD is: is ADHD causing troubles sleeping or vice versa? Are they both symptoms arising from the same physiological disorder, or are they separate but affecting each other? It’s probably a complex answer, with lack of sleep exacerbating symptoms of ADHD (such as hyperactivity or inattention) and ADHD exacerbating difficulties with sleep (Cassoff et. al, 2012).
Furthermore, there’s a difficulty in assessing the impact of medication. Some studies show that medications used to treat ADHD (often stimulants) worsen sleep, while others have been found to have no effect or even improve it (e.g. OROS methylphenidate) (Cassoff et. al, 2012). So, basically, your medication might be making your sleep a lot better, or possibly worse. Or it might have no effect at all. I hope that clears it up.
Children with ADHD tend to have a lot of other comorbidities as well, because the brain is just a poorly put-together hunk of fat that will pile on issues once any little thing goes wrong. Studies have estimated between 9% to 21.2% of people with ADHD are likely also diagnosed with bipolar disorder. The rates of depression among people with ADHD are 24.4 to 31%, anxiety almost 50%, and there are very high rates of substance use disorders among people with ADHD (Hodgins et. al, 2013). Fun stuff! There’s probably a lot of reasons behind this, including a possible genetic component and similar neurobiology. Many hypotheses have been proposed to possibly account for the overlapping between ADHD and other psychiatric disorders (Klassen at. al, 2010):
- The symptoms are similar and thus possibly the criteria to be diagnosed for one disorder is fulfilled by the presence of another.
- The neurobiology behind the overlapping disorders is similar.
- Stimulants used to treat ADHD lead to the development of further issues (if this were a side-effect listed on medication, it would probably be aired in commercials involving women slowly running through a field with a scrolling text describing the possibility of developing depression and BPD).
- This is all random chance (aka psychiatrists can't be fucked to explain it so they shrug their shoulders and go 'Ah, what did you expect. God clearly hates you already.').
- And more!
ADHD and BPD, aka why is ADHD comorbid with everything?
Borderline Personality Disorder, often shortened to BPD, is a mental illness involving severe mood swings, emotional dysregulation and impulsive behaviour. Dysfunctions in systems of neurotransmitters, namely the dopaminergic, serotonergic and adrenergic systems seem to underpin the condition, which is similar to ADHD. There also seems to be a genetic overlap between the two issues (Ditrich et al., 2021).A population analysis by Kuja-Halkola et. al determined that an individual with diagnosed ADHD has a 19.4 times higher risk of having BPD than a non-ADHD person (which is a lot.) Does this mean ADHD leads to higher risk of BPD? Do certain genes cause both disorders? Or are they both different parts of an overarching disorder? All of these explanations and more have been proposed, but we don’t yet really know! It’s likely a whole number of things that includes genetic susceptibility to developing the condition, environmental risk factors, and epigenetic changes resulting from your environment (Ditrich et al., 2021).
Okay. That was another tangent. So we now know that ADHD is comorbid with BPD (and a whole lot more). What about the insomnia you’ve been promised? Don’t worry, we’re getting there. The issue with ADHD being comorbid with a lot of other psychiatric disorders is that a lot of these also tend to cause or exacerbate sleep issues. Boy, this is starting to sound bleak, isn’t is?
Let’s take a break from figures and look at some cool science for a change. We’ve already touched upon the psychological/behavioral explanations behind the relationship between ADHD and BPD, wherein they both exacerbate the other, but what about the actual neurobiology? It's all well and good to talk about them being comorbid, but why are they comorbid? There has to be a reason, we can't just chalk everything up to coincidence! A hypothesis concerning the pairing of these two conditions includes abnormalities in the same brain structures. A study by Nanfang Pan et al. examined the common and divergent anomalies of ADHD/BPD brains. There’s a lot in common so far, but they’re still distinct disorders, so they must be different - and the study found that they definitely all. While a lot of ADHD is characterized by a reduction in volume of certain brain areas and their hypoactivation, BPD involves the hyperactivation of areas related to emotion and instability. The text itself is fascinating, but like a lot of neuroscience articles, hinges on a lot of acronyms, with sentences such as “Coactivation patterns in MACM analysis are shown in Table S5 and Figure S1 , as anomalies of ADHD mainly coactivated with the CEN, while those of BPD linked with the DMN “ (Pan et al., 2023). Which - I mean, Jesus Christ. What do any of those even mean?
In the section discussing “common neural abnormalities among ADHD and BPD”, there’s significant emphasis on dysfunction in the Inferior Parietal Lobe (IPL). The IPL does a whole lot, such as dealing with attention and spatial processing. It also spends a lot of the time feeling dejected because scientists had to call it the "inferior parietal lobe" when, frankly, it's no less important than the so-called superior one, thank you very much. While there were some similarities between the brain structure of people with ADHD and BPD, the study also found a lot of differences. Even if a region was abnormal in a patient with ADHD and the same region was abnormal in a patient with BPD, they were often abnormal in completely different ways! Maybe this doesn’t entirely help explain why ADHD and BPD are comorbid, then? Either way, further study is needed on the brain structure differences in patients ith these conditions. All I’ve really learned is that I hate acronyms with a passion.
Another study hypothesized that differences in the frontostriatal networks and salience/ventral attention networks overlap in ADHD and BPD (Shen et al., 2020). Whoof. Again, those are some complicated names. Remember, kids - if the words don’t appear incoherent at first, it’s not science! 1 Luckily for you, I bit the bullet and did some reading on what the hell those are. The frontostriatal networks are concerned with motor, cognitive and limbic functions (Morris et al., 2016). Boy, you try to explain one word and suddenly you have to explain twenty more, huh? The limbic system is easy to remember, as it concerns the four Fs: feeding, fleeing, fighting and mating.
The frontostriatal networks connect the frontal lobe (this one’s easy - it’s literally the lobe of the brain that’s at the front, concerned with voluntary movement and language) and the basal ganglia (a part of the brain that primarily deals with executing motor control, but is also involved in behavior and emotions). The salience network (SN), also called the ventral attention network is a network comprising many regions of the brain, primarily the temporoparietal junction (TPJ) and the ventral frontal cortex (VFC) which is involved in detecting salient stimuli. Obviously. Right, so what the hell are salient stimuli?
Salient stimuli are just stimuli that attract our attention. They’re something distinct from the rest of the environment. This can be because of bright colors, movement, or a loud noise, for example. If you see a crazed murderer with a machete rushing at you, you probably want to have a way to detect that surprising stimuli, even if the task you’re working on is important and you’re focusing on it. It can probably wait until you’re not at risk of being stabbed. Unfortunately, the salience network also means if you are late and rushing into a lecture, all the heads will probably turn to watch you - not because they’re particularly interested or they’re judging you, but just because you’re sprinting past the seats and panting. Everyone will probably start paying attention to you again when you realize you came late to the wrong lecture and now have to try and slowly make your way back out of the lecture hall. I don’t want to talk about it.
Okay, so there are differences in the frontostriatal networks and salience networks in both ADHD and BPD patients compared to a regular brain. If we think about the symptoms of BPD and ADHD, this might make sense - issues with attention, behavior and regulating emotions are significant for both. Finding the links between different disorders is complicated, and we likely don’t yet really understand the real reasons behind the overlap. An issue I do want to bring up, however, is that BPD (and many of the other disorders commonly found in individuals with ADHD) can also worsen your sleep! Patients with BPD often have insomnia, shortened REM sleep, and suffer from nightmares (Vanek et al., 2021).Therefore, is it possible that people with ADHD who suffer from sleep issues are just struggling with those because of other related disorders? Probably sometimes, but not always. Let’s look into it anyway.
1Note: this is definitely not a good definition for science.
Finally, we're getting somewhere!
We mentioned previously that ADHD is associated with dysfunction in the systems of many neurotransmitters, especially dopamine and norepinephrine/noradrenaline (they’re both the same molecule, but Americans and Brits can’t come to a consensus as to which one to use). These neurotransmitter systems are also implicated in sleep. Remember the ‘sleep switch’: the system is based on mutual inhibition between the VLPO (sleep promoting) and the arousal system (the monoaminergic system, where monoamines are a type of neurotransmitters including dopamine, norepinephrine, epinephrine and serotonin). Therefore, it’s clear that a dysfunction in one of these systems will probably throw your whole sleep schedule off. ADHD is literally a dysfunction of “attention”, and it seems that attention and arousal are both mediated by common systems (e.g. the locus coeruleus is a small collection of neurons in your brainstem with noradrenergic neurons projecting to the central nervous system. Issues with this system of noradrenaline signaling have been implicated in both ADHD and insomnia) (Shen et al., 2020).
Studying the link between ADHD and insomnia can be complicated by factors we’ve mentioned before. Studies should account for use of stimulants to treat ADHD and their effect on sleep, the psychological interplay between the conditions, other diseases comorbid with ADHD which might skew results, and more! Despite this, some very cool research has been conducted. A study by Chun Shen and others has investigated the abnormal brain structures common to both ADHD and insomnia and the genetic correlates. They obtained MRI data from a study by the Adolescent Brain Cognitive Development study, along with information about the ADHD symptoms and sleep disturbances of the children as measured by their parents (Shen et al., 2020).
As a sidenote, sleep disturbances were separated into two categories:
- Dyssomnias - Dyssomnias are disorders impacting the quantity or quality of sleep, and include insomnia or sleep apnea. These are the boring ones (well, okay, not boring per se. They can be severely debilitating to quality of life and overall a terrible experience for anyone impacted. They’re also, in another blow to sufferers, significantly less cool than parasomnias. Sorry).
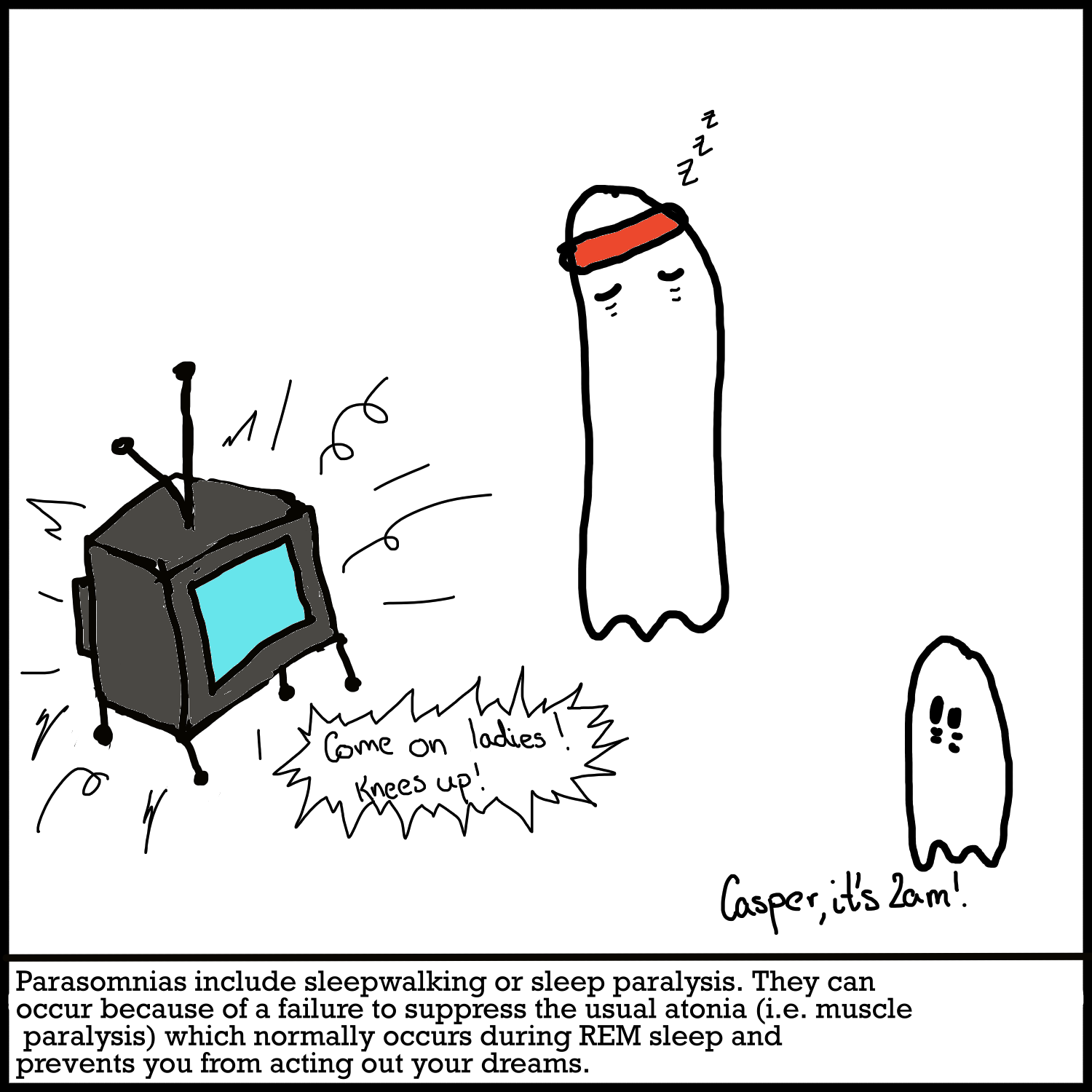
- Parasomnias- these are the weird ones. These sleep disorders are about disrupted sleep - they have all of the cool and terrifyingly-named disorders under their umbrella, like “night terrors”, “recurrent isolated sleep paralysis” and “exploding head syndrome”. (Sidenote: exploding head syndrome is a lot less scary than it sounds. I looked it up. It just means you hear a loud noise in your head when falling asleep or waking up in the night. Still weird, but significantly less terrifying than your head actually spontaneously exploding).
Side-sidenote: Sleep paralysis is a lot creepier and, in my opinion, much cooler. No offense to any sufferers - it sounds terrifying, but from a science point of view, something that could explain why people keep thinking they get abducted and probed by aliens has to be pretty damn cool. Sleep paralysis has gotten to be a pretty popular term. It describes someone suddenly finding themselves unable to move and possibly feeling that there is another presence in the room while they’re asleep or just waking up. It’s an REM disorder (REM being the ‘dreaming’ stage of sleep). It’s probably not a very pleasant experience; in fact, the terrifying feeling of being frozen, visited by a strange being or even floating outside of your own body is often attributed to starting many of the myths about alien abductions, succubi and other common cultural phenomena that make us think of country men with tinfoil hats chewing on a straw and ranting about the government sending 5-dimensional entities to haunt them.
J. Allen Cheyne described three main factors in sleep paralysis:
- Intruder - The feeling that a hostile presence is there. This is a combination of hallucinations and a fear state, presumably precipitated by a state of hypervigilance in the midbrain. This state of hypervigilance can come about due to high stress levels or a disorder such as PTSD; there is strong evidence for the role of orexigenic neurons (which, if you remember, we talked about in terms of narcolepsy). Orexigenic neurons are implicated in both the fear system and sleep.
- Succubus- This is a male succubus. I’d assume that Allen Cheyne chose incubus rather than succubus to fit the alliteration, but I’m going to call this a succubus anyway because I’m a feminist and I support women’s rights and women’s wrongs. this consists of feelings of pressure on the chest and difficulty breathing. In REM sleep, inhibitory motor neurons reduce your rate of respiration (Xie, 2012). Since you’re not really moving around (well, unless you suffer from a parasomnia) and being as active as when you’re awake (again, unless something is a bit off), it’s logical not to need so much oxygenation. This decrease in respiration and your respiratory muscles being inhibited could contribute to the Succubus symptomology. Why people have interpreted it as a demon stealing in through their windows to have sex with them, I’m not entirely certain. I’m not a psychologist. Go ask your parents. Or your teachers. Or maybe the internet.
- Unusual body experiences:- They just completely gave up on the alliteration here. Why not “Irregular corporeal incidents”, or “intriguing bodily instances”? Honestly, this kind of thing is what puts people off science. I’ll give it to them in that unusual body experiences is pretty easy to comprehend - it’s the classic out-of-body experiences or feeling like you’re floating. This one is pretty interesting to consider the reason behind, and I can’t cover it in much detail without making this tangent far too long - and frankly, there’s not that much research to be found on the subject! The current hypotheses tend to focus on the fact that the lack of control over muscles during REM sleep while the simultaneous ‘awakening’ of the sensory system probably contribute to a whole range of strange sensations. We also have the vivid REM dreams melting through the fabric of your sleep to soak your normal reality. Some cool research has considered the role of mirror neurons - for more on this, see Sleep Paralysis, “The Ghostly Bedroom Intruder” and Out-of-Body Experiences: The Role of Mirror Neurons. A more philosophical person might think about this in the context of our perception of self and our ego. Luckily for you, I don’t have the critical reasoning skills for any of that, so I’m just going to move on!
I’ve gotten all tangled up in another tangent. You know how I called this section “Finally, we’re getting somewhere”? Lies. Again. So for real:
But actually this time
Let’s circle back to the study by Chun Shen and her group, the MRI and genetic study of children with ADHD and sleep disorders. The neuroimaging study was conducted to determine whether ADHD and sleep disturbances did, as hypothesized, share common “neural correlates” (Shen et al., 2020). The study writes: “Among these clusters, we found 3 overlapping areas, including in the bilateral insula, left caudate, and putamen (2762 voxels); in the right middle frontal gyrus and inferior frontal gyrus (2296 voxels); and in the right parahippocampus, hippocampus, and amygdala (419 voxels)”. As always when reading scientific papers, what an absolutely terrifying sentence. However, if you’ve been reading the rest of the website (and I can’t blame you if you haven’t - I talk a lot), you’ve probably come across some of these terms before. (If you’re asking what a voxel is, I looked it up. A voxel is a tiny unit building up the 3D image of the brain in an fMRI. Like a pixel, but… volatile? Voluptuous? I don’t know why they used a v.)
The study goes on to specify ADHD and dyssomnias (the category that includes insomnia) were associated with gray matter reductions in the right frontal gyrus, bilateral insula, left striatum, right amygdala and hippocampus.
The frontal gyrus we’ve mentioned as one of the overlapping areas in the MRIs of ADHD and sleep disordered brains; this part has been implicated in impulse control and inhibitory motor control (El-Baba & Schury, 2023). The bilateral insula (bilateral meaning it’s on both sides of the brain) is a structure dealing with cognition and motivation. It’s similar to the amygdala in terms of dealing with emotion, but while the amygdala does a more basic, automatic processing of those emotions, the insula deals with subjective processing of emotions. Insular deficits have been implicated in many psychiatric conditions - for example, activity in the insula was found to be decreased in patients with major depressive disorder. Additionally, degeneration in the insula has been found to be linked to the loss of sense of self in patients with Alzheimer’s (Namkung et al., 2017). Clearly, the insula is a pretty important lil bit of your brain. Then we have the left striatum - we talked about the striatum in the “Treatment” section of ADHD. The striatum is one of the main parts of the brain amphetamines act on; it’s part of the basal gangli and helps coordinate movement and has other, probably more relevant functions in the reward cascade. We’re almost there! The amygdala is the fear-processing system; it’s the 4 F’s one. It’s part of the limbic system and does a whole bunch of stuff: a lot of emotional responses, memory and decision making. And last but not least, the hippocampus - we can think of this as the memory one. These neural circuits are related to networks that we’ve mentioned before - the frontostriatal networks and salience/ventral attention system. We've talked about these in terms of ADHD and BPD comorbidity, but they are likely implicated in dyssomnias as well. These networks mediate aspects of cognition and attention, which are both implicated in the pathophysiology of ADHD and insomnia. Disturbances in sleep are related to issues with arousal, while ADHD is related to deficiencies in attention. Attention and arousal are closely linked and both modulate each other. One study described it as the connections between ‘generators’ of attention and the sensory areas which process them being indirectly modulated via the arousal system based on the “reticular activating system” (a bundle of nerves in your brain stem) (Coull, 1998).
As expected, the Chun Shen study found overlapping neurotransmitter pathways between ADHD and dyssomnias. Most notably, these were in “subcortical regions” - these include some of the structures we’ve discussed such as the hypothalamus or amygdala. We can thus make some assumptions about possible treatment - if medication for ADHD targets the neurochemical signaling pathways which also cause dyssomnias, we’d be killing two birds with one stone (isn’t this a weird idiom? Who’s out here hunting birds with stones? Why isn’t it two birds with one shot? Two birds with one arrow? Or maybe something less violent, like hug two friends with one arm. Pet two puppies with a single hand. A lot of these are starting to hinge on not having all limbs. I also have to admit I had to look up the difference between a proverb and an idiom).
One study by Melanie Furrer et al. looked at control people with no ADHD, unmedicated ADHD-ers and medicated peeps. We’ll call them the Cs, Us and Ms. No we won’t. That’s dumb. We’ll call them the controls, unmedicated and medicated. The study examined the relationship of ADHD and stimulants to slow-wave EEG sleep activity. Slow-wave sleep is considered the deepest form of sleep, it being the hardest to wake people from. It’s a form of NREM sleep, the non-dreaming sleep. One interesting little fact is that the main brain regions undergoing slow-wave activity shifts as you age, moving “posterior to anterior” (from the back of the brain to the front). In children with ADHD, slow-wave sleep is found in more central parts of the brain, similar to children of a younger age, likely reflecting the disruptions in cortical maturity of ADHD. In the unmedicated group, there was less gray matter and a delay in frontal cortical development. Slow-wave activity was decreased by 20.5% across the head in ADHD patients compared to controls - a very significant amount! An analysis, accounting for any differences in age, was done specifically on medicated vs unmedicated ADHD people. Slow-wave sleep was still reduced in people who had taken stimulant medication in the past but were not taking it currently, but seemed to have normalized in patients who were taking medication. This was parallel to a normalization in their gray matter volume and the thickness of their cortical region. However, there are a lot of confounding factors and limitations to be discussed. For example, slow-wave EEG activity also depends on the activities someone does during the day, and on the length of time which the individual spent awake prior (Furrer et al., 2019). Furrer’s study incorporated sleep diaries which didn’t find significant differences in when people went to bed or woke up, therefore implying that differences in time spent awake shouldn’t have accounted for the decrease in slow-wave EEG. Additionally, what if the ADHD subgroups just had poorer sleep because they had issues such as restless leg syndrome or sleep apnea? Obviously if you have sleep apnea and you stop breathing frequently during the night, your sleep won’t be particularly restful. To account for this, the study excluded people known to suffer from these sleep disorders and the study didn’t find differences in awakenings or sleep-wake history as would otherwise be expected. At least in this study, it therefore seems that treating ADHD can lead to significant improvements in at least some aspects of sleep - good news!
To circle back to the Chen Shun study looking at common neurology between ADHD and dyssomnias, the authors mention that there are aspects of sleep issues which don’t seem to stem from ADHD symptoms or don’t have common neurological correlates. Therefore, we clearly need to take a broader view in terms of treatment. Treating either will likely help the other (unless the stimulants have the unlucky effect of increasing arousal), with better sleep lessening ADHD symptoms and ADHD medication seeming to decrease sleep issues.
Treatment and future prospects
I hope it’s clear from my long-winded and often barely comprehensible summary that there’s still a lot more research to be done. When looking at a person with ADHD and insomnia, it’s easy to see and attempt to treat those issues separately, but that might not be the best mode of action. But Kaja, I hear you say, there’s so many ways to sleep better! What about taking melatonin supplements? What about just not using your phone in bed? My Aunt’s mother’s cousin’s neighbor said that she had great results when she went on a smoothie detox and flushed all the sleep-inhibiting toxins from her body. Well, you guys can go on a smoothie detox, but I’m going to pass. That sounds miserable. Also, please stop protesting. Having voices in my head constantly is making me go crazy. I can’t think. I can’t sleep! That might just be the ADHD/insomnia, actually.
Let’s look at melatonin. Melatonin is a hormone released by the pineal gland in response to darkness. It tells the suprachiasmatic nucleus that it’s time to start sleeping. But, as we already know, it’s far from the only thing that would make us sleep. After all, if darkness and melatonin was all we needed, we wouldn’t be staying awake through the night - we’d all just conk out in the evenings. Clubs would be frequented far less and would probably be significantly cleaner as a result. Dark, sketchy alleyways would be a great place for naps. Melatonin can be very useful in treating jet-lag; after all, this isn’t a condition where your sleep is out of whack because you’re stressed or your sleep switch isn’t quite working, but it happens because you’ve moved to a new area and your brain still needs a bit of time to adjust to the new light-dark cycle. However, studies seem to mostly agree that melatonin can treat insomnia only “to a limited extent” (Costello et al., 2014).
What about benzodiazepines? Often called just benzos, they’re a group of CNS depressants that act as GABA agonists, causing the same inhibitory effect that GABA exerts. This causes its sedative and hypnotic effects, and its role as a sleep aid. Studies have found benzos to decrease sleep latency (a fancy way of saying how long it takes someone to fall asleep) and increased the actual duration of sleep - but the big drawback here was that these studies were short-term, in that they only investigated the changes for 14 days (Lie et al. 2015). Are there negative side-effects to taking them long-term? Short answer: Yup. Longer answer: Tolerance can build up relatively quickly. The benzodiazepines quickly lose their ability to potentiate the GABA-A receptor because the receptors are downregulated, leading to a person needing to use a lot more of the drug to get the same effect. Additionally, there’s not a lot of substantial evidence that benzodiazepines actually do help in the long-term (Guina & Merrill, 2018)! Doctors are much less likely to prescribe benzodiazepines today, with some favoring a first-course treatment of looking at the comorbidities of the patient and establishing a healthy sleep routine. Of course, this might not still be enough, but it’s probably better than chronic usage of benzodiazepines. One study found that not only was chronic benzodiazepine usage associated with less slow-wave sleep and reduced sleep efficiency, but in patients who were withdrawing from benzos, their sleep efficiency (how long they actually slept compared to how long they spent in bed) was pretty much the same once they were off benzodiazepines and had gone through withdrawal as it was on the drugs (Poyares et al., 2004). Plus, they can have some side-effects such as confusion, drowsiness, unsteadiness and more. If you want to learn a bit more about how benzodiazepines work, you can look at this page and watch a video or two: Benzodiazepine information
What about pharmacological treatments that aren’t benzodiazepines? I’m so happy to talk about these - not because they’re particularly incredibly, but because I really hate spelling benzodiazepines. Benzodiazapenes? Benzodiazepenes? Who the hell knows. Spell-check, apparently. And I’m tired of getting corrected every thirty seconds. The big alternatives are called “Z drugs” (significantly easier to spell). They act on the same GABA-A receptors as benzodiazepines, have a pretty quick onset and a relatively short half-life. This means that they (hopefully) shouldn’t affect you the next day as much as benzodiazepines (although the side-effects beg to differ), but also they might not significantly increase sleep time. They seem to work better than benzodiazepines and are often viewed as safer (Agravat, 2018). But - and you can see a trend emerging here - they don’t come without their own problems. They’re safer in many ways than benzodiazepines, but still have potential for issues such as respiratory depression and confusion or dizziness. Additionally, they’re acknowledged to be addictive when used chronically and potentially cause withdrawal symptoms (Agravat, 2018). And, yet again, there is a lack of information on their long-term effects.
The treatment of choice for insomnia is typically cognitive behavioral therapy. While sleep medications can be given, they’re usually only used in the short-term as we’ve discussed. Drugs can be easy to build up a dependance to. That’s not to say medications can’t be helpful, but more that currently, they’re not a feasible long-term solution. Very few studies have actually empirically studied the effect of cognitive behavioral therapy (often shortened to CBT, or CBT-i for insomnia) on ADHD patients. A 2019 Swedish study gave patients 10 weekly 90 minute CBT-i sessions, with adjustments made for ADHD. They found that insomnia severity improved “significantly” and that even ADHD symptoms were improved at a 3-months follow-up. The CBT-i was adjusted to ADHD patients somewhat, with emphasis given on keeping a sleep routine, organizing strategies were given in the first session, and there were more shorter sessions rather than fewer longer ones (Jernelöv et al., 2019). Of course, this might not really have helped at all, because there’s not really any studies to compare this with. Even this study was just a small pilot study - clearly, more research has to be done on a larger scale. If any billionaire with a well-stocked lab and lots of research groups is reading this and thinking “Gosh, I sure hope I stumble upon something that I could start funding that is as of yet under researched”, well boy are you in luck!
There’s other treatments that are in the works, and plenty we have yet to come up with. Light therapy is one of these (I mean, it’s one of the alternative treatments, not that it’s a treatment we have yet to come up with||). It’s quite literally what it sounds like - using light in an attempt to reset your circadian rhythm. This has been found to be “effective” in treating sleep issues (van Maanen et al., 2016), but it only targets the circadian aspect of your sleep regulation, and as we know (because I keep repeating it), there’s a whole lot more to sleep and sleep disorders. Still, it’s definitely beneficial in that unlike pharmacological treatments, it doesn’t have the same side-effects caused by long term potentiation of CNS receptors. It’s literally just having specific light shone indirectly in your eyes - quite difficult to build up a dependency to (van Maanen et al., 2016).
Unfortunately, aside from these, the big advice that you can really get is the regular advice: don’t use screens in bed, expose yourself to light once you wake up, try and set regular sleep/wake up times, and try and get psychiatric help if you feel either your ADHD or your insomnia is negatively impacting your quality of life. Boring stuff, I know - but it’s the best I got. For now. Until someone develops a cool pill you can swallow to just conk out and fall asleep. And not ina coma-inducing way, but a proper, restful night’s sleep. In my vision of the future, therapy has gotten to the point where we intimately understand insomnia and comorbidities. If I feel anxious, I simply think to myself: “No I don’t.” With a heavy head, I fall back onto the pillows. I snuggle into my covers. My legs don’t feel restless. I’m not worried about getting enough sleep because I know I will. I lie back and drift off. Goodnight!
References
- Fadeuilhe, C., Daigre, C., Richarte, V., Grau-López, L., Palma-Álvarez, R. F., Corrales, M., & Ramos-Quiroga, J. A. (2021). Insomnia Disorder in Adult Attention-Deficit/Hyperactivity Disorder Patients: Clinical, Comorbidity, and Treatment Correlates. Frontiers in psychiatry, 12, 663889. https://doi.org/10.3389/fpsyt.2021.663889
- Coull, J. T. (1998). Neural correlates of attention and arousal: Insights from electrophysiology, functional neuroimaging and psychopharmacology. Progress in Neurobiology, 55(4), 343–361. https://doi.org/10.1016/s0301-0082(98)00011-2
- van Maanen, A., Meijer, A. M., van der Heijden, K. B., & Oort, F. J. (2016). The effects of light therapy on sleep problems: A systematic review and meta-analysis. Sleep Medicine Reviews, 29, 52–62. https://doi.org/10.1016/j.smrv.2015.08.009
- Agravat, A. (2018). ‘Z’-hypnotics versus benzodiazepines for the treatment of insomnia. Progress in Neurology and Psychiatry, 22(2), 26–29. https://doi.org/10.1002/pnp.502
- Jernelöv, S., Larsson, Y., Llenas, M., Nasri, B., & Kaldo, V. (2019). Effects and clinical feasibility of a behavioral treatment for sleep problems in adult attention deficit hyperactivity disorder (ADHD): A pragmatic within-group pilot evaluation. BMC Psychiatry, 19(1). https://doi.org/10.1186/s12888-019-2216-2
- Poyares, D., Guilleminault, C., Ohayon, M. M., & Tufik, S. (2004). Chronic benzodiazepine usage and withdrawal in insomnia patients. Journal of Psychiatric Research, 38(3), 327–334. https://doi.org/10.1016/j.jpsychires.2003.10.003
- Guina, J., & Merrill, B. (2018). Benzodiazepines I: Upping the care on downers: The evidence of risks, benefits and alternatives. Journal of Clinical Medicine, 7(2), 17. https://doi.org/10.3390/jcm7020017
- Lie, J. D., Tu, K. N., Shen, D. D., & Wong, B. M. (2015). Pharmacological Treatment of Insomnia. P & T : a peer-reviewed journal for formulary management, 40(11), 759–771.
- Furrer, M., Jaramillo, V., Volk, C., Ringli, M., Aellen, R., Wehrle, F. M., Pugin, F., Kurth, S., Brandeis, D., Schmid, M., Jenni, O. G., & Huber, R. (2019). Sleep EEG slow-wave activity in medicated and unmedicated children and adolescents with attention-deficit/hyperactivity disorder. Translational Psychiatry, 9(1). https://doi.org/10.1038/s41398-019-0659-3
- Costello, R. B., Lentino, C. V., Boyd, C. C., O’Connell, M. L., Crawford, C. C., Sprengel, M. L., & Deuster, P. A. (2014). The effectiveness of melatonin for promoting healthy sleep: A rapid evidence assessment of the literature. Nutrition Journal, 13(1). https://doi.org/10.1186/1475-2891-13-106
- El-Baba, R. M., & Schury, M. P. (2023, May 29). Neuroanatomy, frontal cortex. NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK554483/
- Namkung, H., Kim, S.-H., & Sawa, A. (2017). The insula: An underestimated brain area in clinical neuroscience, psychiatry, and neurology. Trends in Neurosciences, 40(4), 200–207. https://doi.org/10.1016/j.tins.2017.02.002
- Morris, L. S., Kundu, P., Dowell, N., Mechelmans, D. J., Favre, P., Irvine, M. A., Robbins, T. W., Daw, N., Bullmore, E. T., Harrison, N. A., & Voon, V. (2016). Fronto-striatal organization: Defining functional and microstructural substrates of behavioural flexibility. Cortex, 74, 118–133. https://doi.org/10.1016/j.cortex.2015.11.004
- Morin CM, Jarrin DC, Ivers H, Mérette C, LeBlanc M, Savard J. Incidence, Persistence, and Remission Rates of Insomnia Over 5 Years. JAMA Netw Open. 2020;3(11):e2018782. doi:10.1001/jamanetworkopen.2020.18782
- Efron D, Lycett K, Sciberras E (2014) Use of sleep medication in children with ADHD. Sleep Med 15:472–475. doi:10.1016/j.sleep.2013.10.018
- Owens JA. Sleep disorders and attention-deficit/hyperactivity disorder. Curr Psychiatry Rep. 2008 Oct;10(5):439-44. doi: 10.1007/s11920-008-0070-x. PMID: 18803919.
- Cassoff, J., Wiebe, S. T., & Gruber, R. (2012). Sleep patterns and the risk for ADHD: a review. Nature and science of sleep, 4, 73–80. https://doi.org/10.2147/NSS.S31269
- Hodgkins, P., Setyawan, J., Mitra, D. et al. Management of ADHD in children across Europe: patient demographics, physician characteristics and treatment patterns. Eur J Pediatr 172, 895–906 (2013). https://doi.org/10.1007/s00431-013-1969-8
- Klassen LJ, Katzman MA, Chokka P. Adult ADHD and its comorbidities, with a focus on bipolar disorder. J Affect Disord. 2010;124(1–2):1–8. doi: 10.1016/j.jad.2009.06.036.
- Ditrich, I., Philipsen, A., & Matthies, S. (2021). Borderline personality disorder (BPD) and attention deficit hyperactivity disorder (ADHD) revisited – a review-update on common grounds and subtle distinctions. Borderline Personality Disorder and Emotion Dysregulation, 8(1). https://doi.org/10.1186/s40479-021-00162-w
- Kuja-Halkola R, Lind Juto K, Skoglund C, Rück C, Mataix-Cols D, Pérez-Vigil A, et al. Do borderline personality disorder and attention-deficit/hyperactivity disorder co-aggregate in families? A population-based study of 2 million swedes. Mol Psychiatry.2021; 26(1):341–9. https://doi.org/10.1038/s41380-018-0248-5.
- Pan, N., Wang, S., Qin, K., Li, L., Chen, Y., Zhang, X., Lai, H., Suo, X., Long, Y., Yu, Y., Ji, S., Radua, J., Sweeney, J. A., & Gong, Q. (2023). Common and distinct neural patterns of attention-deficit/hyperactivity disorder and borderline personality disorder: A multimodal functional and structural meta-analysis. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, 8(6), 640–650. https://doi.org/10.1016/j.bpsc.2022.06.003
- Shen, C., Luo, Q., Chamberlain, S. R., Morgan, S., Romero-Garcia, R., Du, J., Zhao, X., Touchette, É., Montplaisir, J., Vitaro, F., Boivin, M., Tremblay, R. E., Zhao, X.-M., Robaey, P., Feng, J., & Sahakian, B. J. (2020). What is the link between attention-deficit/hyperactivity disorder and sleep disturbance? A Multimodal examination of longitudinal relationships and brain structure using large-scale population-based cohorts. Biological Psychiatry, 88(6), 459–469. https://doi.org/10.1016/j.biopsych.2020.03.010
- Xie A. (2012). Effect of sleep on breathing - Why recurrent apneas are only seen during sleep. Journal of thoracic disease, 4(2), 194–197. https://doi.org/10.3978/j.issn.2072-1439.2011.04.04
Contact Me
E-mail: kkubickova03@gmail.com